The Kentucky-centered outbreak of the rare E. coli O103 strain infects 72 people in five states, according to the federal Centers for Disease Control and Prevention (CDC) in Atlanta.
Eight people with the outbreak strain have been hospitalized, the CDC report says. No cases of the hemolytic uremic syndrome (HUS) or deaths have been reported.
CDC says the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS), the U.S. Food and Drug Administration (FDA), and several states are also involved in the ongoing investigation.
The probe has yet to identify a specific food item, grocery store or restaurant that is responsible for the outbreak.
CDC’s report, coming shortly before noon on Friday, was the first information released by the federal agency since Kentucky officials a week earlier disclosed the outbreak occurrence.
“This is a rapidly evolving investigation,” CDC said. “We will update our advice if a source is identified.”
People infected with the outbreak strain of E. coliO103, by state of residence, as of April 4, 2019 (n=72)
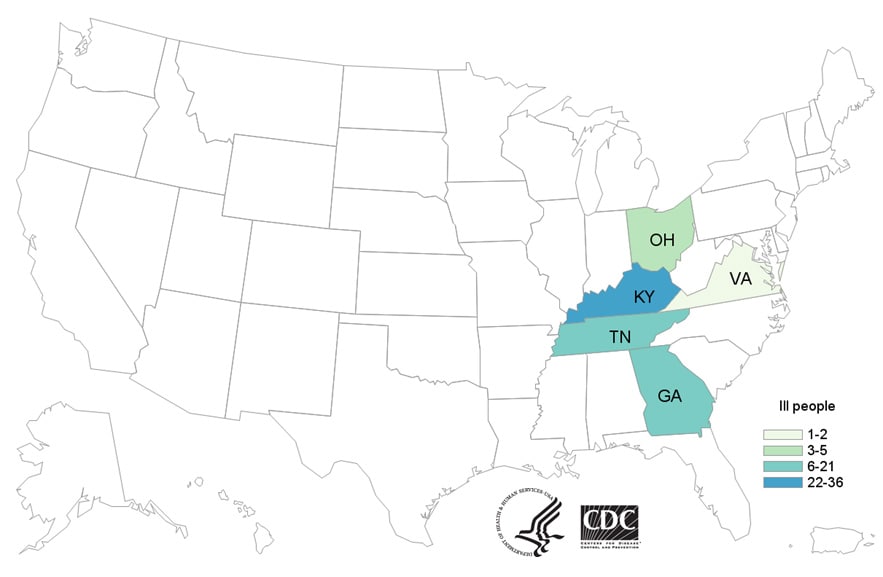
Illness from the outbreak strain occurred from March 2 to 29, 2019. People infected range in age from 1 to 74 years, with a median age of 17. CDC finds 55 percent are female. From those available to provide information, eight or 17 percent required hospital care.
CDC’s case count of 72 is current as of April 4, 2019. Public health investigators are using the PulseNet system to identify illnesses that may be part of the outbreak. PulseNet is the national subtyping network of public health and food regulatory agency laboratories coordinated by CDC.
DNA fingerprinting is performed on E. coli bacteria isolated from ill people by using techniques called pulsed-field gel electrophoresis (PFGE) and whole genome sequencing (WGS).
CDC PulseNet manages a national database of these DNA fingerprints to identify possible outbreaks. WGS gives a more detailed DNA fingerprint than PFGE. WGS performed on E. coli from ill people in this outbreak showed that they are closely related genetically.
“This means that the ill people are more likely to share a common source of the illness,” CDC concluded.
Advice From CDC for Consumers, Restaurants, and Retailers
Take action if you have symptoms of an E. coli infection:
- Talk to your healthcare provider.
- Write down what you ate in the week before you started to get sick.
- Report your illness to the health department.
- Assist public health investigators by answering questions about your illness.
Follow these general ways to prevent E. coli infection:
- Wash your hands. Wash hands after using the restroom or changing diapers, before and after preparing or eating food, and after contact with animals.
- Cook meats thoroughly to kill harmful germs. Cook steaks and roasts to at least 145˚F and let rest for 3 minutes after you remove meat from the grill or stove. Cook ground beef and pork to at least 160˚F. Use a food thermometer to check the temperature of the meat.
- Don’t cross-contaminate food preparation areas. Thoroughly wash hands, counters, cutting boards, and utensils after they touch raw meat.
- Wash fruits and vegetables before eating, unless the package says the contents have been washed.
- Avoid raw milk, other unpasteurized dairy products, and unpasteurized juices.
- Don’t prepare food or drink for others when you are sick.
Symptoms of E. coli Infection
- People usually get sick from Shiga toxin-producing E. coli (STEC) 2–8 days (average of 3–4 days) after swallowing the germ.
- Some people with a STEC infection may get a type of kidney failure called hemolytic uremic syndrome (HUS).
- E. coli infection is usually diagnosed by testing a stool sample.
- Antibiotics are not recommended for patients with suspected E. coliinfections until diagnostic testing can be performed and E. coli infection is ruled out. Some studies have shown that administering antibiotics to patients with E. coli infections might increase their risk of developing HUS, and a benefit of treatment has not been clearly demonstrated.
- For more information, see Symptoms of E. coli Infection.
(To sign up for a free subscription to Food Safety News, click here.)

