Foodborne illnesses have long been suspected of leading to Crohn’s disease, a chronic inflammatory bowel disease (IBD).
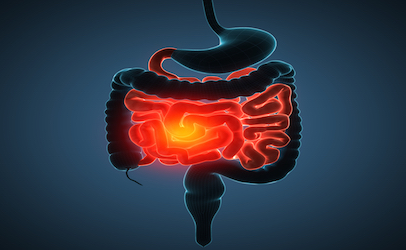
An immune response to tissue injury has been known to causes redness, swelling and pain in the digestive or gastrointestinal (GI) tract with the potential for also threatening the mouth, esophagus, stomach, small and large intestines, and anus.
Crohn’s can affect any part of the GI tract, from the mouth to the anus, but it is more commonly found at the end of the small intestine. This is the area where the large intestine or colon begins.
 New research published in the Oct. 6, 2016 edition of PLOS/Pathogens confirms that exposure to foodborne pathogens causing acute gastroenteritis does produce a long-term risk of Crohn’s disease “well into the post-infectious period but the mechanistic basis for this ongoing relationship to disease onset is unknown.”
New research published in the Oct. 6, 2016 edition of PLOS/Pathogens confirms that exposure to foodborne pathogens causing acute gastroenteritis does produce a long-term risk of Crohn’s disease “well into the post-infectious period but the mechanistic basis for this ongoing relationship to disease onset is unknown.”
About 700,000 people suffer from Crohn’s annually in the U.S., and its an equal opportunity disease impacting men and women at about the same rates. Symptoms range from mild to severe. And while Crohn’s can strike at any age, most people experience onset in the 15 to 35 age range. Also 20 percent of people with Crohn’s have a relative who also has the disease.
The new research entitled “Acute Infectious Gastroenteritis Potentiates a Crohn’s Disease Pathobiont to Fuel Ongoing Inflammation in the Post-Infectious Period” was funded by grants from the Canadian Institutes of Health Research and Crohn’s and Colitis Canada.
The researchers say adherent-invasive E. coli are among the bacteria that has been linked to Crohn’s, with several laboratories having reported a higher prevalence of E. coil in Crohn’s patients compared to healthy subjects.
The E. coli are said to share an “evolutionary ancestry” with extraintestinal pathogenic E coli. Crohn’s is more common in individuals exposed to infectious gastroenteritis caused by Salmonella and other enteric pathogens, “sometimes with onset times on the order of years after the infectious episode,” the researchers reported.
They found infectious gastroenteritis increases the risk of Crohn’s; that gastroenteritis causes inflammation that selectively disrupts the resident intestinal microbiota; and intestinal infections are a probable cause of relapse for inflammatory bowel disease patients.
Their work came to conclusion that E. coli colonized in the gut is a modifier to response to acute infectious gastroenteritis.
(To sign up for a free subscription to Food Safety News, click here.)
